Peanut Balls for Better Birthing (For Patients and Nurses)
If a patient asked you what the one item they’ll want by their side in labor, you might think of a few objects. Maybe a phone comes to mind, a printed birth plan, or a stress ball. At the Birth Nurse, our #1 tool for trauma-informed birthing are peanut balls. They may look and sound funny, but they offer serious benefits for birthers and nurses. Let’s get into why peanut balls make for better birthing.
As an L&D nurse, you’ve seen beautiful moments and painful ones as well. You’re witness to turning points in people’s lives; the moment when a couple becomes a family, when a new baby enters the world, when a person becomes a parent. You also see tragedy, and those moments stay with you. You’re a key player in the stories that families will tell for decades.
And, as a nurse, you have the power to change these stories. Using your toolkit of L&D skills, you can alter outcomes and make the birthing process better for patients.
Every pregnancy has its risks, and pain is an inevitable side of birth. But what if a few simple tools could help you give your patients a shorter, less painful labor? What if you could change a woman’s birthing story from 36 hours of pain to just a few minutes of pushing? What if you could be the nurse that patients talk about for the next lifetime as “that amazing labor nurse who knew just what to do”?
Every nurse can be that special caregiver for patients. And peanut balls are the first step in a nurse’s journey in trauma-informed birthing care. When you add peanut ball education to your L&D toolkit, you make yourself a more effective patient advocate and a more confident clinician. But first, I should probably introduce myself…
Hi There, I’m the Birth Nurse!
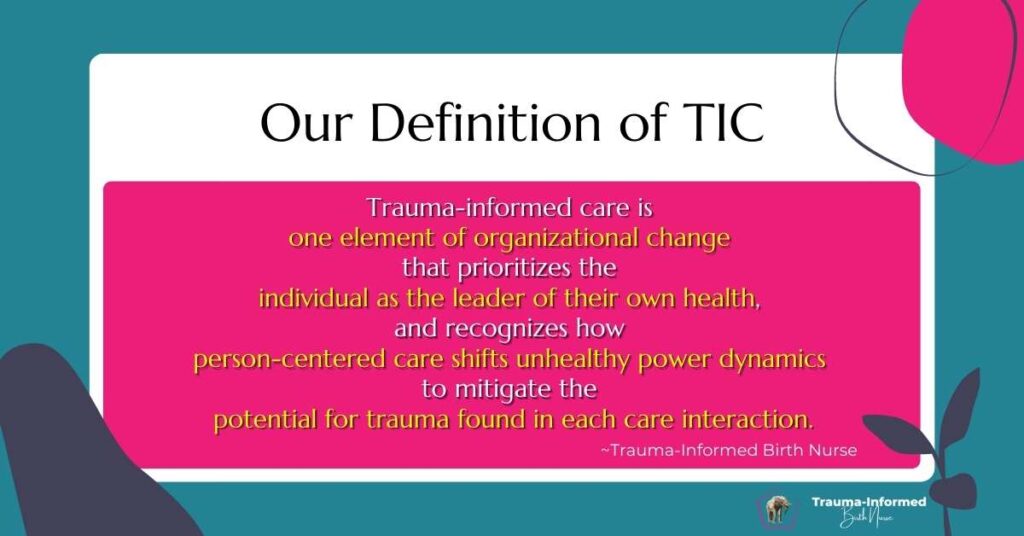
My name is Mandy Irby, and I head up a team of labor clinicians who are passionate about making care better for birthers and nurses. We teach individual nurses and whole nursing units the principles and paradigm shift of trauma-informed care (TIC).
Maybe you’ve heard of TIC before, and maybe you’ve been confused by it. TIC is a growing standard in medicine, yet many clinicians still don’t understand what it means or the difference it makes in practice. At its heart, the TIC framework helps clinicians give patients autonomy, shared decision-making, and respect.
But you don’t just flip a switch or take one CE to be a trauma-informed birth nurse. It’s a journey of discovery and re-understanding our roles as care advocates.
On the individual level, becoming trauma-informed helps you feel more empowered and allows you to give patients more respectful care. On the unit level, implementing a trauma-informed framework helps units meet AIM bundle goals, reduce cesarean rates and unnecessary interventions, and prevent trauma.
The start of the trauma-informed journey is peanut balls. These silly-sounding (but powerful) tools help us as nurses give patients more options. Many L&D nurses can point to a closet full of peanut balls gathering dust on their unit. You might know you should be using them, yet you don’t know why or how. And with no one else using them on your unit, they must not be that necessary, right?
By the end of this article, you’re going to know exactly why peanut balls are our #1 labor tool. Let’s get into when you might need the peanut ball labor tool and how they help in different stages of labor.
How Peanut Balls Help With Labor
Nurses who understand the power of peanut balls can educate and bring better outcomes to patients and units. Growing research has shown that peanut balls help measurably improve cesarean rates, tearing, laboring time, and more.
Peanut Balls Prevent Unnecessary C-Sections
Cesarean deliveries are associated with more risks to the birther and baby, yet they’ve only gotten more common in the last several years. Needless c-sections put patients at risk for infection, hemorrhage, uterine rupture, problems with later placental implantation, and the need for a hysterectomy.[1] And while there are several indications that prevent a vaginal birth, many cesareans are unnecessary.
In 2020, nearly one in three births in the United States happened via cesarean delivery.[2] A patient’s likelihood of getting a c-section has a lot to do with the hospital they go to for care and the obstetric unit culture. There’s a huge difference in cesarean rates among facilities, with some only at 7.1% and others at nearly 70%.[3] This discrepancy in care doesn’t have to exist.
The good news is that peanut balls help prevent unnecessary c-sections by about 12%.[4] Peanut balls help open the birth canal and shift the fetal position to promote natural labor. By arming yourself with tools to lower cesarean rates, you can make birth safer in your whole unit.
Even in birthers who are slowed by epidural and failure to progress, peanut balls make a vaginal birth more likely. Let’s talk about how peanut balls are a vital tool for when patients meet Failure to Progress (FTP).
Peanut Balls Counteract Failure to Progress
Failure to Progress is the most common indicator for primary cesarean deliveries.[5] This can be related to epidurals, weak contractions, fetal placement, and a small pelvic canal. One of the first recommendations in FTP is movement, yet epidurals prevent most forms of independent positioning. Clinicians have few tools at hand when a patient’s labor stalls, which makes the perceived only solution a cesarean delivery.
Peanut balls have been shown to hasten the first stage of labor by 90 minutes on average and cut the second stage in half.[6] Unlike standard birthing balls, birthers who can’t move their legs can still use them without extra support. They help patients dilate more quickly and help drop the fetus lower. Peanut balls also help prevent fetal heart rate irregularities, as well as the need for instrumental birth and fetal malposition, as they relate to FTP.[7][8]
Because peanut balls help the fetus descend in the pelvis, they also help with the birther’s comfort through nonpharmacological pain reduction.
Peanut Balls Offer Patient Comfort and Pain Reduction During Labor
Pain related to birth may seem inevitable, and L&D nurses believe they have few options to present to patients. Discomfort in labor is directly related to patient anxiety and affects labor outcomes and birthing experiences. Peanut balls help reduce discomfort related to fetal positioning and contractions without impeding labor progression.5
Peanut balls are an essential tool in an L&D nurse’s nonpharmacological toolkit. Not only do they help prevent cesarean delivery, but they also help move birth along faster and with less pain. Arming yourself with peanut ball training helps you feel more confident in birthing care. Now let’s talk about how effective peanut balls are for whole units.
Peanut Balls Are an Essential Tool in Labor & Delivery Units
Peanut balls are proven to make labor faster, less painful, and less risky. But they’re only as effective as the nurse who educates patients about them. And it takes confidence in your own skills to bring a bright pink peanut ball into a patient’s room and offer to put it between their legs. Peanut balls help units meet core safety standards, give patients a better birth experience, improve unit culture, and make nurses more confident in care.
Peanut Balls Help Meet Essential Care Standards
Peanut balls help improve unit and nursing care with these tracked standards:
- NTSV (nulliparous, term, singleton, vertex) cesarean deliveries are tracked by the Joint Commission (JCAHO).[9] This measure reflects the quality of perinatal care for first-time birthers and will be publicly published. Hospitals that do not invest in reducing high cesarean rates risk losing accreditation if they can’t meet JCAHO standards.
- The Centers for Medicare and Medicaid (CMS) will soon be tracking new electronic quality measures (eCQMs) for perinatal care. Starting in 2024, cesarean birth and severe obstetric complications will be charted and tracked alongside safe opioid use in obstetrics. These measures will be reported publicly and will affect hospital and unit funding.
- Every AIM safety bundle includes care that is respectful, equitable, and supportive. The AIM cesarean reduction bundle specifically notes the need for unit culture that “values, promotes, and supports spontaneous onset and progress of labor and vaginal birth.” Peanuts balls help nurses and units do just that.
As an individual nurse, it’s easy to feel powerless working within hospital systems. So much of patient care isn’t up to you. But learning about peanut balls can help you improve your unit’s metrics in these specific, measurable ways.
There’s another measurable standard that peanut balls can improve; patient satisfaction scores.
Peanut Balls Improve Patient Satisfaction
Nurses who help patients use the peanut ball give them more options in their care. Traditional pushing in stirrups isn’t comfortable, and it’s not associated with the best outcomes. Yet it’s the default option on most L&D units because it suits providers. True patient-centered care gives autonomy to patients rather than demanding that they suit the preference of clinicians.
Peanut balls help patients feel empowered because they can choose the position that feels right for them. Peanut balls give patients dozens of different positioning options and help patients have a better birthing experience as a whole. In research, patients have been so satisfied with their experience with peanut balls that 71% would recommend them to other birthers. Patients have reported that peanut balls helped them be more comfortable, sped labor, and helped them position.[10]
L&D units that emphasize patient autonomy using the peanut ball can give patients better experiences and improve their HCAHPS scores as a result. Peripartum care makes up a larger percentage of hospital stays than any other inpatient specialty.[11] Improving patient satisfaction in obstetrics units has a positive impact on hospitals as a whole.
But how does peanut ball training affect clinical staff? We can’t talk about patient care and leave out the essential L&D nurses that make it possible.
More Tools = More Confident Nurses
Peanut balls help nurses feel like experts in patient care. Peanut ball training helps you, as a provider, feel more confident and equipped when a patient turns to you and asks, “What now?”
How would it feel to be the nurse that knows the exact right solution when a patient is failing to progress? Wouldn’t you be proud of yourself if you knew that you’d prevented an unnecessary (and unwanted) c-section? Nurses feel more confident in their care abilities when they have more tools in their toolkits. And learning about peanut balls can also help you change your unit as a whole.

Trauma-Informed Care Improves Unit Culture
Peanut balls are a gateway to unit-wide trauma-informed care principles. Consistent peanut ball usage helps nurses offer patient-centered care, which doesn’t just make medicine better for patients. Units that understand the core principles of respect and autonomy also improve whole-unit culture, which makes coming to work better.
With all of the benefits that peanut balls offer, do most hospitals have them?
Do Hospitals Provide Peanut Balls?
Every hospital should have peanut balls to support labor. But not every unit culture emphasizes them, and not every nurse knows how to educate patients about them. If you’re a practicing nurse who doesn’t have much experience with peanut balls, don’t feel bad! We can fix this.
Maybe your unit hasn’t used peanut balls much because it’s easier to stick to old ways than to do something new. Maybe you’ve got a few seasoned nurses who bring them out once in a while, but you don’t have the confidence to educate a patient on them yourself.
You know that changing practices from “the old ways” can be a slow process. But you can be the change agent on your unit by educating yourself on peanut balls and helping your peers get educated as well.
Let’s talk about how to get started with peanut balls so that you can start using this essential tool in your next labor.
Peanut Ball Training: How to Get Started
If reading this article has made you curious about peanut balls and how you can help patients use them, we’re so glad! The Birth Nurse educates nurses like you in trauma-informed tools so you can offer the best birthing care possible and feel great doing it.
We offer live peanut ball training for L&D nurses who are beginners and intermediate. Our training includes on-demand remote sessions, as well as a workbook, pdf guide to use during your shift, and options for continuing education. Our goal is to see you succeed at implementing this care into your practice.
To learn more about this unique course and the powerful skills you’ll come away with, check out our peanut ball training page. We want to see you using peanut balls for better birthing practices in your unit, and that starts with you.
Psst… If you want to learn more about peanut balls, and do it on your unit’s dime, share this article and our peanut ball flier with your unit leadership.
References
[1] The Joint Commissions. (2021, April 7). Promoting safer cesarean delivery. The Joint Commission. Retrieved February 8, 2023, from https://www.jointcommission.org/resources/news-and-multimedia/blogs/leading-hospital-improvement/2021/04/promoting-safer-cesarean-delivery
[2] Centers for Disease Control and Prevention. (2023, January 31). FastStats – Births – method of delivery. Centers for Disease Control and Prevention. Retrieved February 7, 2023, from https://www.cdc.gov/nchs/fastats/delivery.htm
[3] Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood). 2013 Mar;32(3):527-35. doi: 10.1377/hlthaff.2012.1030. PMID: 23459732; PMCID: PMC3615450.
[4] Grant, C., & Clutter, L. (n.d.). The Peanut Ball: A Remarkable Labor Support Tool. DONA International.
https://premierbirthtools.com/wp-content/uploads/2014/11/PeanutBallArticleInternationalDoula2014.pdf
[5] Gifford DS, Morton SC, Fiske M, Keesey J, Keeler E, Kahn KL. Lack of progress in labor as a reason for cesarean. Obstet Gynecol. 2000 Apr;95(4):589-95. doi: 10.1016/s0029-7844(99)00575-x. PMID: 10725495.
[6] Tussey, C., & Botsios, E. (2011). Use of a labor ball to decrease the length of labor in patients who receive an epidural. Journal of Obstetric, Gynecologic & Neonatal Nursing, 40. https://doi.org/10.1111/j.1552-6909.2011.01243_25.x
[7] Tussey CM, Botsios E, Gerkin RD, Kelly LA, Gamez J, Mensik J. Reducing Length of Labor and Cesarean Surgery Rate Using a Peanut Ball for Women Laboring With an Epidural. J Perinat Educ. 2015;24(1):16-24. doi: 10.1891/1058-1243.24.1.16. PMID: 26937158; PMCID: PMC4748987.
[8] Kamath P, Pai M, Shenoy R, Karkada S, D’souza S, Noronha J. Effectiveness of a peanut ball device during labour on maternal and neonatal outcomes: protocol for a randomised controlled trial. F1000Res. 2022 Nov 21;11:717. doi: 10.12688/f1000research.109537.2. PMCID: PMC9727314.
[9] NTSV Cesarean Birth Overview. NTSV Cesarean Birth Overview | California Maternal Quality Care Collaborative. (n.d.). Retrieved February 8, 2023, from https://www.cmqcc.org/focus-areas/quality-improvement/ntsv-c-sections#:~:text=This%20measure%20is%20known%20as,no%20breech%20or%20transverse%20positions
[10] Payton, C.L. (2015). Use of the Peanut Ball to Decrease First and Second Stages of Labor.
[11] McDermott, K. W., Elixhauser, A, Sun, R. (2017, June). Trends in Hospital Inpatient Stays in the United States,
2005–2014. Retrieved 26 May 2019, from U.S. Department of Health and Human Services, Agency for Health Care Research and Quality, Healthcare Cost and Utilization Project Website:
https://www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.pdf



5 Responses
Explore Labor and Delivery Nurse CME Conferences, Meetings, and Online CME Courses. Register for upcoming 2023 Labor and Delivery Nurse Conferences & earn CME Credits