Hey, Hi, Hello!
We’re educators passionate about protecting patients and clinicians from birth-related trauma. Our founder, Mandy Irby, started the Birth Nurse after going through vicarious trauma as a delivery nurse and her own birthing trauma. We fiercely believe in protecting birthers from trauma as they bring new life into the world. We’re also passionate clinician advocates who arm nurses and the birth team with tools to protect themselves from vicarious trauma.
We educate individual parents and nurses in trauma informed birth care. But we also know that the biggest change happens at the system and state levels. That’s why we’ve got 55 hospital partners and counting. We want to help your unit or hospital by giving your staff the best in trauma informed birthing care education.
When we talk to administrative leaders, many haven’t heard of this type of clinician education. Yet this training will be essential in the birthing care model of the future. Hospitals implementing this education will enjoy ROIs in patient satisfaction, staff retention, and enhanced safety bundle adherence. And that’s just the tip of the iceberg.
Here are eight reasons every hospital should offer trauma informed birth care training to their care teams. Units who’ve completed trauma informed birth care training:
- Improve patient satisfaction scores on HCAHPS by prioritizing the birther as the decision-maker.
- Earn the “Birthing Friendly” designation, setting their system apart from competitors.
- Increase adherence to AIM safety bundles that improve hospital- and state-measured goals.
- Decrease costs associated with patient safety events, like unnecessary cesarean deliveries.
- Improve maternal safety, protecting birthers from downstream effects of trauma.
- Improve clinician safety and retention, and save on costs related to turnover and burnout.
- Boost unit coordination, communication, and safety culture on the whole-unit scale,
- Step into the future of birthing care.
Curious about how one program can do all this for your unit or system? Let’s get into the evidence behind why this training is so effective.
Trauma Informed Care Increases Patient Satisfaction
The birthing process is a critical time for patients to experience the hospital and the system at large. A family’s experience during childbirth can influence their decision to pursue pediatric and adult care at the same facility. Birthers are often family decision-makers for children and older adults, and their experiences determine where their family will get care.
The peripartum period makes up a larger percentage of hospital stays than any other specialty by far.[1] Improving the patient experience in birthing and neonatal units is critical for hospitals to maintain patient retention and reimbursement for services. Of recently discharged patients, more than 1/5th are postpartum people. Improving satisfaction rates in this specialty can benefit Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores more than in any other.[2]
Yet patient satisfaction during the peripartum period can leave much to be desired. Traumatic experiences do not lead to good patient satisfaction. In the 2018 Listening to Mothers Survey in California, four in ten women reported that a provider tried to induce their labor before they were comfortable. 75% of those who felt pressured to induce went ahead despite their fears.[3]
Provider-centered care hurts patient satisfaction. Another example of this is how birthers in the states have historically been put into stirrups during active labor. The most current research has shown that this position isn’t the safest or most comfortable for birthers, yet this remains the standard practice in most hospitals.[4]
Under trauma informed care, this type of pressure is obstetric violence. Clinicians in our training are educated with tools that help them empower patients. Trauma informed methods do not include pressuring birthers to induce before they’re ready, or requiring them to use a position that isn’t comfortable for them.
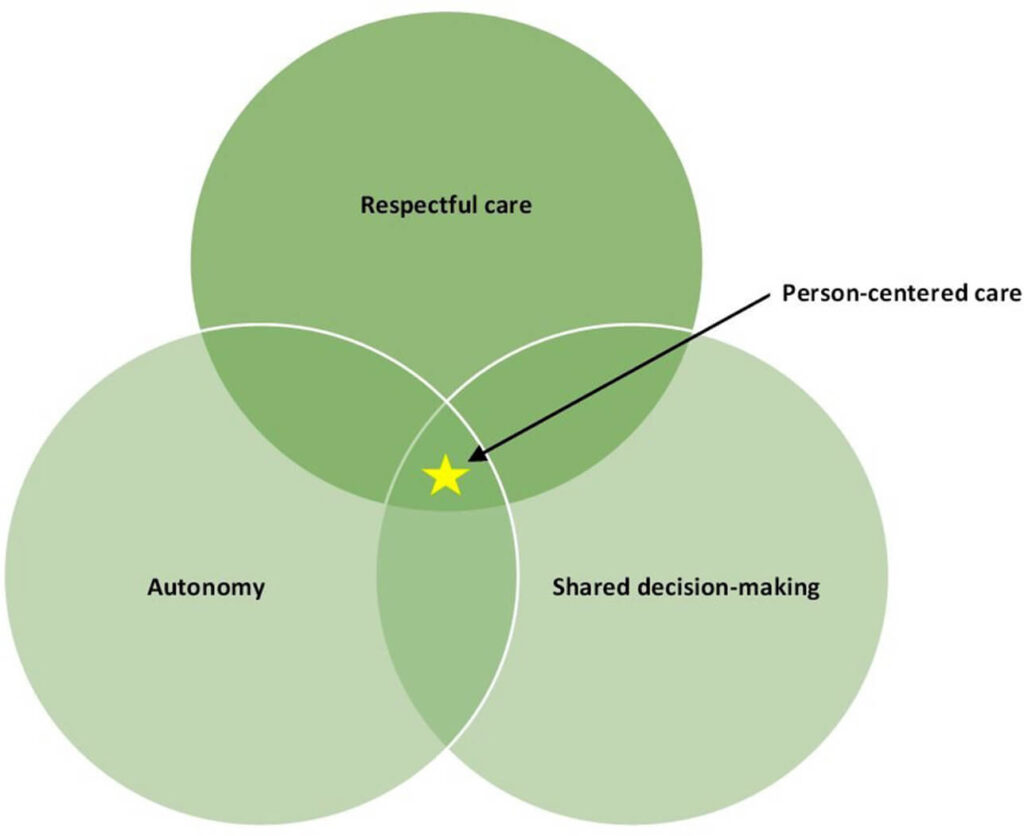
Trauma informed care improves patient experiences by making patients the center of care. We help care teams implement shared decision-making. This helps patients be autonomous and allows clinicians to deliver respectful care. The result is care that is truly patient-centric.
Rather than their decisions being dictated by what makes providers comfortable, birth care that recognizes trauma puts the patient at the helm. Patients are more satisfied when they get to dictate their care, and HCAHPS results increase.
This cutting-edge training puts hospitals and systems ahead of the curve, while others still use outdated methods that traumatize patients and put more pressure on providers. And there’s a special new designation for hospitals that prioritize birthing care. Let’s talk about it.
The “Birthing Friendly” Designation
In December 2021, the White House issued a national call to action to reduce maternal mortality and morbidity rates in the United States. The US has long had some of the highest maternal illness and death rates among high-income nations. Among minority populations, these rates are even higher due to systemic racism and discrimination. In 2020, the rate of death for Black birthers was found to be three times the rate for white birthers, and had risen from 2019.[6]
In 2023, the Department of Health and Human Services (DHHS) will establish a separate, publicly-reported hospital designation for hospitals prioritizing maternal health outcomes. The Centers for Medicare & Medicaid Services (CMS) have released a guidance memo that encourages hospitals to implement the following:[7]
- Evidence-based best practices for managing obstetric emergencies
- Interventions to address factors that contribute to maternal health disparities
To support these changes, the Biden-Harris administration plans to establish a “Birthing-Friendly” designation through the 2023 President’s Budget. This public-facing hospital designation reflects investments in the quality and safety of maternal care. The first-of-its-kind quality designation will set hospitals apart for families looking for birthing care.
This is good news for birthing families, who will soon have more ways to evaluate a hospital or birthing unit before going in for care. But it also means hospitals that don’t pursue safer, higher-quality birth care may soon find fewer families coming to them. The good news is trauma informed birthing care training checks off both boxes.
Trauma informed care training helps care teams communicate better with patients and each other in emergencies. It also helps providers establish a baseline of trust. And many of the factors that contribute to health disparities are associated with implicit bias.[8] By helping clinicians understand differences in care and the trauma they can cause, our training improves marginalized maternal care.
Trauma informed birth training also fits into existing safety bundles. Let’s talk about which bundled care measures can improve after implementing this training.
Measurable Improvements to AIM Patient Safety Bundles
Bundled care programs help hospitals improve care processes and outcomes. The Alliance for Innovation on Maternal Health (AIM) tracks adherence to standardized care bundles. Some specific bundles even have state-tracked metrics, allowing public health authorities to track more complex outcomes, such as maternal mortality.
Our program fits within several AIM safety bundles and increases adherence to specific patient safety measures. Our program helps hospitals adhere to every maternal care bundle because this education helps units provide respectful, safe care. Here are a few specific ways our program helps units and hospitals consistently implement bundled care:
- Every AIM safety bundle requires respectful, equitable, and supportive care. This requires every team member to communicate openly, transparently, and empathetically with patients. Peripartum persons must be key decision-makers in their care. Their unique values and goals must be reflected in the shared goals of the care team. In addition, patients have the right to respectful refusal. All of these requirements are met within trauma informed care training.
- The AIM obstetric hemorrhage bundle requires additional staff support for patients who refuse blood products. It also requires further review of the root causes of disparities in hemorrhage care. Pre-birth education ensures patients understand the signs and risks of birth. Trauma-informed training helps clinicians understand and respect patients’ decisions for blood treatments and encourages more thorough education to address these bundle goals.[9]
- The AIM cesarean reduction bundle requires units to build a culture that “values, promotes, and supports spontaneous onset and progress of labor and vaginal birth.” Under trauma informed care, patients aren’t pressured to induce or undergo a cesarean without indication, which is an immediate requirement of this safety bundle. We help units maximize the likelihood of safe vaginal birth while using shared decision-making processes to reduce unnecessary and unwanted c-sections.[10]
Our training helps units adhere to AIM safety bundles in more ways than one. That’s because our one-stop unit programs help teams develop as a whole. To improve whole-patient safety, you have to educate the whole unit. But what impact does this program have on costs related to adverse safety events? Here’s how trauma informed training helps units save on patient safety costs.

Trauma Informed Training Decreases Patient Safety Costs
Adverse safety events in the hospital are linked to greater care costs and higher spending during the acute care period and after discharge.[11] Trauma informed training helps reduce the costs associated with adverse safety events in the OB setting. It also decreases the psychological trauma that birthing events can cause for patients and families.
Birth can be risky, and some of these risks are impossible to control. A study published in 2022 found that the most common triggers for safety events in birthing care weren’t maternal health but problems within health systems. Researchers noted that better training in team communication could reduce these health events and hospital spending.[12]
For example, cesarean delivery rates have increased substantially in the last few decades. Yet we know that C-sections are associated with worse safety and efficacy for birthers and infants.[13] C-sections are associated with tripled rates of severe maternal morbidities, compared to vaginal deliveries.[14] Education for parents and clinicians has strongly shown to decrease these rates.[15]
For example, our training helped Iowa hospitals decrease safety-related costs by preventing unnecessary c-sections. In 2020, their cesarean delivery rates were projected to rise by 2%. But after we trained 200 of their staff in a live, virtual workshop, their cesarean delivery rates decreased by 2%.[16]
From a risk management perspective, harm reduction training is a win-win. Administrators can decrease safety events and the associated costs, while clinicians feel safer under the trauma informed care model. Let’s talk about the impacts of trauma informed birth training on patient outcomes.
Trauma Informed Care Increases Patient Safety
Traumatic experiences can be mitigated with education, support, culture shifts, and proper care. Yet they happen more often than they should. Nearly half of first-time mothers experience trauma during their birthing experience. Rates of PTSD after birth trauma are up to 18.5% in high-risk groups.[17],[18]
To make matters worse, previous trauma makes women more vulnerable to traumatic birthing experiences. Sexual abuse survivors are more likely to be re-traumatized during birth. Women with prior mental health diagnoses and poor relationships with their providers are also at higher risk.[19],[20]
When we think about the consequences of psychological trauma, PTSD is the first diagnosis that comes to mind. Of pregnant, birthing, and postpartum people, 9% have a diagnosis of PTSD.[21] But this isn’t the only downstream effect for people with traumatic childbirth experiences. Here’s a list of other associated effects of birthing trauma:
- Risk for problems with breastfeeding[22]
- Increased risk for postpartum depression[23]
- Increased risk for psychosis and anxiety[24]
- Increased risk for emergency cesarean delivery[25]
- Increased risk for postpartum hemorrhage
Traumatic experiences during birth cause harm to patients in more ways than one. This quote by birthing trauma researchers puts this point beautifully:
“The few minutes or hours that a woman perceived she has been traumatized during birth can be likened to a pebble dropped into a pond resulting in ripples spreading out in the water.”
-Beck, Watson & Gable, 2018[26]
To protect birthers from the downstream safety effects of birthing trauma, hospitals need to arm clinicians. Research has shown that higher feelings of control and self-determination mitigate the long-term health effects of trauma.[27] We help nurses prioritize patients as leaders in their own care, helping them shift the power dynamic so that patients are more in control.
Trauma informed care training increases patient safety by preventing and mitigating psychological trauma at the unit, hospital, and system levels.[28] Hospitals that invest in this training can help prevent trauma in birthers and families.[29] But this training doesn’t just help patients. It also arms nurses with tools to protect themselves from secondary trauma, and mitigates burnout in the process. Let’s get into how our program impacts birth unit nurses.
Improvements in Nurse Safety & Retention
Clinician trauma has risen exponentially in the last several years because of increased awareness and more burden on providers. Secondary trauma, vicarious trauma, and second-victim rates have skyrocketed since COVID-19. Risks are higher amongst less experienced clinicians, who may suffer from:11
- Burnout
- PTSD
- Depression
- Substance abuse
- Suicide
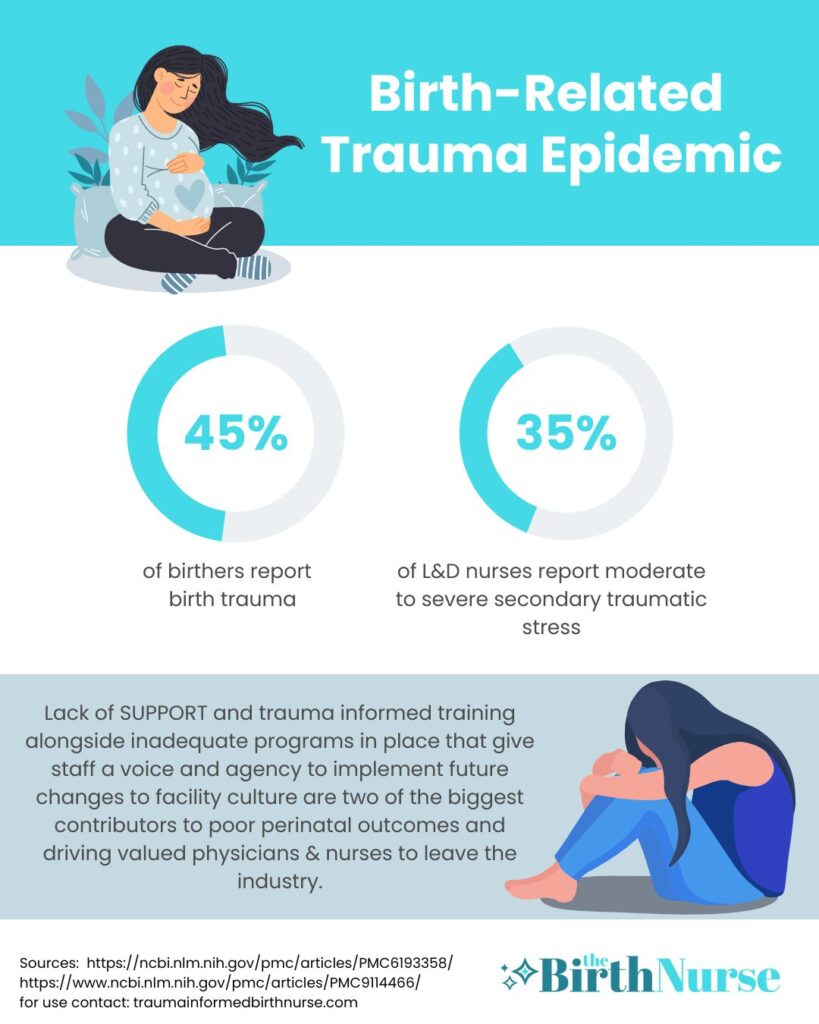
Within the obstetrics field, losses can be especially devastating for staff.[30] Of maternal-newborn nurses, 24-29% experience secondary trauma symptoms.[31] The most common of these are intrusive thoughts, sometimes called flashbacks. Secondary trauma is preventable at the system scale. Because hospitals don’t address it, vicarious trauma and moral injury continue to push nurses out of the bedside.[32]
We don’t need to tell you about the exodus that healthcare is experiencing because of these conditions. A 2022 survey found that a third of nurses were planning to leave their positions because of burnout and stress.[33] And the more clinicians leave, the worse conditions are for those that stay – accelerating the burnout process.
This process of systemic trauma and burnout is a massive cost for hospitals and healthcare systems. One report found that the average hospital spends over $16k per nurse annually on costs associated with burnout. That’s just for the nurses that stay.[34] On average, the cost of turnover per nurse is estimated at over $46,000.[35]
Our training helps mitigate turnover rates related to clinician trauma and burnout in birthing units. Trauma informed care training helps protect clinicians from secondary trauma and gives them resources to feel empowered in their own practice. Research has shown that providing nurses the trauma informed lens has many benefits, such as:[36]
- Enhancing satisfaction at work
- Reducing their risk for burnout
- Helping them give patients better experiences and outcomes
Trauma informed education helps hospitals proactively prevent clinician burnout, rather than relying on hollow “self-care” promotions. Pamphlets, pizza parties, and signs about burnout are nonspecific and don’t address the root causes of burnout. To protect clinicians and hospitals, we need to give clinicians better resources around trauma and stress. Trauma informed birthing care helps nurses stay in the patient care setting and reduces nurse turnover in obstetrics units.
Your investment in our training extends far beyond the live education we provide. We also give nurses ongoing connection through our private, self-paced professional development space. Our growing community of over 60 nurses can help support your team. And we have a robust learning library of continuing education that doesn’t require any additional commitment from units or hospitals.
Nurses aren’t the only clinicians negatively impacted by trauma and turnover. Physicians and other clinicians are leaving the bedside because of poor support and high stress in acute care. Let’s talk about how our birth training helps interprofessional team members protect themselves and communicate for better patient care.
Impacts on Interprofessional Clinician Engagement & Communication
Trauma informed birth training isn’t just for nurses! Nurses aren’t the only clinicians impacted by secondary trauma. And isolating this training to “just nurses” can lead to gaps in patient experiences. That’s why we arm whole units with these tools using interdisciplinary birthing education.
Interdisciplinary education is rapidly becoming a standard for training, not only for nurse education but for physicians, PAs, NPs, and unlicensed staff. Safety culture can only be established through communication across licenses and professions. Small-group training that includes interprofessional team members has been shown to reinforce a culture of safety and communication between team members.[37]
Trauma informed birth training is a simple, one-stop program that arms nurses and allied professionals with key tools they’ll use for the rest of their lives. Training nurses, physicians, APPs, and unlicensed staff at once promotes collaboration, communication, and enhanced patient outcomes.[38] Not to mention, interprofessional education is considerably cheaper. It’s just more efficient to educate professionals together than to arrange individual sessions for each group.
When we arm whole teams with the tools of trauma informed care, everybody wins. Nurses, Physicians, APPs, and unlicensed staff love our programs because we help them practice without compromising their ethics. Clinicians who go through our training get the benefits of feeling more confident in patient care. Here’s what one clinician had to say after going through our trauma informed birth care training:
“This course has been showing me the full dimensionality of what trauma looks like in our specialty. This is useful in connecting with patients and to keep from being complicit in causing harm to the patients who place their trust in us to keep them safe.”
Jennifer, RN Review
Our education is unique because it’s an entirely new way of looking at the birth process. Clinicians are empowered under the trauma informed model. By reducing secondary trauma for the whole birthing team, patients get better experiences, better care and outcomes.
This model is rapidly changing how maternal care is delivered. We aim to improve the safety and experiences of patients and help clinicians practice better. Trauma informed birth care is the way of the future. Let’s talk about what that future will look like.
Trauma Informed Care Is the New Standard for Clinicians’ Continuing Education
Trauma informed care may sound like it’ll lead to drastic changes, and some clinicians may resist these shifts. Growing pains are normal. But just because changing from the old ways is hard doesn’t mean it shouldn’t be done. In fact, the history of trauma within the obstetrics specialty means this type of training isn’t just essential – it’s long overdue.
The OBGYN field has some of the highest rates of discrepancies in care for minorities. It’s clear that the differences in health outcomes aren’t because of physiological differences but of how our medical establishments treat minority birthers.[39] Systems that claim to prioritize care for people of color, birthers, and mothers must seek education to begin to dismantle the systems of oppression within the birthing field.
Trauma informed care is essential within a system that values patient autonomy, respectful care, and shared decision-making. Systems that don’t implement trauma informed care training will continue to perpetuate:

- Loss of autonomy
- Dehumanization
- Traumatization
- Obstetric violence
- The long-lasting effects of birth trauma
But don’t just listen to us on all this. In committee opinion, the American College of Obstetricians and Gynecologists have twice recommended that hospitals implement trauma informed care training.[40] The Journal of Obstetrics, Gynecology, and Neonatal Nursing released clinical practice guidelines that detail requirements for respectful maternal care in 2022.[41] Trauma informed training is rising in residency programs, and 100% of residency program directors agree this training should be required within the field.[42]
Yet it’ll take implementation on the system scale for these recommendations to be carried out. Hospitals and units that implement trauma informed birth training equip their staff with better tools to care for patients and protect themselves. They also help diminish disparities in maternal care head-on.
What Every Unit Leader Should Know About Trauma Informed Birth Training
As you can probably tell, we’re really passionate about trauma informed birth training. Trauma informed care is a powerful, system-altering approach to care. It’s understandable for clinicians, administrators, and unit leaders to be intimidated by the changes this model entails.
The one thing we want you to know about this training is that your system can do it too. Yes, this approach will change the way birth units approach patients and their care. And you already know that in medicine, new best practices can be slow to implement, even with the best evidence. But with the help of passionate educators, your whole unit can reap the benefits of trauma informed birth training. Your unit can truly step into the future of trauma informed birth care.
Here at The Birth Nurse, we proudly offer evidence-based education for birthing units wanting to improve the way they treat patients and their staff. If you want to learn more about our cutting-edge training, check out our hospital partners page. And if you’re ready to see how we can help you meet your patient care goals, book your discovery call with our founder, Mandy Irby.
References
[1] McDermott, K. W., Elixhauser, A, Sun, R. (2017, June). Trends in Hospital Inpatient Stays in the United States,
2005–2014. Retrieved 26 May 2019, from U.S. Department of Health and Human Services, Agency for Health Care
Research and Quality, Healthcare Cost and Utilization Project Website:
https://www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.pdf (2014 data)
[2] Nationalpartnership.org. (2015, March). The Priority of Developing and Implementing CAHPS Maternity Care Facility, Clinician and Health Plan Surveys.
[3] Data Snapshot: Listening to mothers in California. California Health Care Foundation. (2020, August 5). Retrieved December 27, 2022, from https://www.chcf.org/publication/data-snapshot-listening-mothers-california/
[4] Huang J, Zang Y, Ren LH, Li FJ, Lu H. A review and comparison of common maternal positions during the second-stage of labor. Int J Nurs Sci. 2019 Jun 20;6(4):460-467. doi: 10.1016/j.ijnss.2019.06.007. PMID: 31728401; PMCID: PMC6839002.
[5] Breman, R. B., Resnick, B., Ogbolu, Y., Dada, S., & Low, L. K. (2022). Reliability and Validity of a Perinatal Shared Decision-Making Measure: The Childbirth Options, Information, and Person-Centered Explanation. Journal of Obstetric, Gynecologic & Neonatal Nursing, 51(6), 631–642. https://doi.org/10.1016/j.jogn.2022.08.001
[6] Centers for Disease Control and Prevention. (2022, February 23). Maternal mortality rates in the United States, 2020. Centers for Disease Control and Prevention. Retrieved December 28, 2022, from https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2020/maternal-mortality-rates-2020.htm
[7] Centers for Medicare and Medicaid Services. (2022, August 1). Fact sheet FY 2023 hospital inpatient prospective payment system (IPPS) and Long Term Care Hospitals (LTCH PPS) final rule – CMS-1771-F maternal health. CMS. Retrieved December 28, 2022, from https://www.cms.gov/newsroom/fact-sheets/fy-2023-hospital-inpatient-prospective-payment-system-ipps-and-long-term-care-hospitals-ltch-pps-1
[8] Wang E, Glazer KB, Sofaer S, Balbierz A, Howell EA. Racial and Ethnic Disparities in Severe Maternal Morbidity: A Qualitative Study of Women’s Experiences of Peripartum Care. Womens Health Issues. 2021 Jan-Feb;31(1):75-81. doi: 10.1016/j.whi.2020.09.002. Epub 2020 Oct 14. PMID: 33069559; PMCID: PMC7769930.
[9] Alliance for Innovation on Maternal Health. (2022, November 30). Obstetric hemorrhage. AIM. Retrieved December 28, 2022, from https://saferbirth.org/psbs/obstetric-hemorrhage/
[10] Alliance for Innovation on Maternal Health. (2022, July 19). Safe reduction of primary cesarean birth. AIM. Retrieved December 28, 2022, from https://saferbirth.org/psbs/safe-reduction-of-primary-cesarean-birth/
[11] Tessier L, Guilcher SJT, Bai YQ, Ng R, Wodchis WP. The impact of hospital harm on length of stay, costs of care and length of person-centred episodes of care: a retrospective cohort study. CMAJ. 2019 Aug 12;191(32):E879-E885. doi: 10.1503/cmaj.181621. PMID: 31405834; PMCID: PMC6690827.
[12] Hüner B, Derksen C, Schmiedhofer M, Lippke S, Janni W, Scholz C. Preventable Adverse Events in Obstetrics-Systemic Assessment of Their Incidence and Linked Risk Factors. Healthcare (Basel). 2022 Jan 4;10(1):97. doi: 10.3390/healthcare10010097. PMID: 35052261; PMCID: PMC8775914.
[13] Srinivas SK, Fager C, Lorch SA. Evaluating risk-adjusted cesarean delivery rate as a measure of obstetric quality. Obstet Gynecol. 2010 May;115(5):1007-1013. doi: 10.1097/AOG.0b013e3181d9f4b6. PMID: 20410776; PMCID: PMC4167363.
[14] Obstetric Care Consensus No. 1. (2014). Obstetrics & Gynecology, 123(3), 693–711. https://doi.org/10.1097/01.aog.0000444441.04111.1d
[15] Chen I, Opiyo N, Tavender E, Mortazhejri S, Rader T, Petkovic J, Yogasingam S, Taljaard M, Agarwal S, Laopaiboon M, Wasiak J, Khunpradit S, Lumbiganon P, Gruen RL, Betran AP. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2018 Sep 28;9(9):CD005528. doi: 10.1002/14651858.CD005528.pub3. PMID: 30264405; PMCID: PMC6513634.
[16] Irby, M. (n.d.). Corporate Case Study. The Birth Nurse. Retrieved December 27, 2022, from https://mandyirby.com/.
[17] Alcorn KL, O’Donovan A, Patrick JC, Creedy D, Devilly GJ. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol Med. 2010 Nov;40(11):1849-59. doi: 10.1017/S0033291709992224. Epub 2010 Jan 11. PMID: 20059799.
[18] Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J Affect Disord. 2017 Jan 15;208:634-645. doi: 10.1016/j.jad.2016.10.009. Epub 2016 Oct 27. PMID: 27865585.
[19] LoGiudice JA. A Systematic Literature Review of the Childbearing Cycle as Experienced by Survivors of Sexual Abuse. Nurs Womens Health. 2017 Dec 2016 – Jan;20(6):582-594. doi: 10.1016/j.nwh.2016.10.008. PMID: 27938798.
[20] Simpson M, Catling C. Understanding psychological traumatic birth experiences: A literature review. Women Birth. 2016 Jun;29(3):203-7. doi: 10.1016/j.wombi.2015.10.009. Epub 2015 Nov 10. PMID: 26563636.
[21] Vignato, J., Georges, J.M., Bush, R.A., Connelly, C.D., 2017. Post-Traumatic stress disorder in the perinatal period: a concept analysis. J. Clin. Nurs. 26 (23–24), 3859–
3868. doi:10.1111/jocn.13800.
[22] Beck CT, Watson S. Impact of birth trauma on breast-feeding: a tale of two pathways. Nurs Res. 2008 Jul-Aug;57(4):228-36. doi: 10.1097/01.NNR.0000313494.87282.90. PMID: 18641491.
[23] Dekel, S., Ein-Dor, T., Dishy, G.A. et al. Beyond postpartum depression: posttraumatic stress-depressive response following childbirth. Arch Womens Ment Health 23, 557–564 (2020). https://doi.org/10.1007/s00737-019-01006-x
[24] Rodríguez-Almagro J, Hernández-Martínez A, Rodríguez-Almagro D, Quirós-García JM, Martínez-Galiano JM, Gómez-Salgado J. Women’s Perceptions of Living a Traumatic Childbirth Experience and Factors Related to a Birth Experience. Int J Environ Res Public Health. 2019 May 13;16(9):1654. doi: 10.3390/ijerph16091654. PMID: 31085980; PMCID: PMC6539242.
[25] Abdollahpour, S., Mousavi, S.A., Motaghi, Z. et al. Prevalence and risk factors for developing traumatic childbirth in Iran. J Public Health 25, 275–280 (2017). https://doi.org/10.1007/s10389-016-0783-y
[26] Beck CT, Watson S, Gable RK. Traumatic Childbirth and Its Aftermath: Is There Anything Positive? J Perinat Educ. 2018 Jun;27(3):175-184. doi: 10.1891/1058-1243.27.3.175. PMID: 30364308; PMCID: PMC6193358.
[27] Elliot AJ, Turiano NA, Infurna FJ, Lachman ME, Chapman BP. Lifetime trauma, perceived control, and all-cause mortality: Results from the Midlife in the United States Study. Health Psychol. 2018 Mar;37(3):262-270. doi: 10.1037/hea0000585. Epub 2018 Jan 25. PMID: 29369676; PMCID: PMC6057153.
[28] Hall, S., White, A., Ballas, J., Saxton, S. N., Dempsey, A., & Saxer, K. (2021). Education in trauma-informed care in maternity settings can promote mental health during the COVID-19 pandemic. Journal of Obstetric, Gynecologic & Neonatal Nursing, 50(3), 340–351. https://doi.org/10.1016/j.jogn.2020.12.005
[29] Hall S, White A, Ballas J, Saxton SN, Dempsey A, Saxer K. Education in Trauma-Informed Care in Maternity Settings Can Promote Mental Health During the COVID-19 Pandemic. J Obstet Gynecol Neonatal Nurs. 2021 May;50(3):340-351. doi: 10.1016/j.jogn.2020.12.005. Epub 2021 Jan 9. PMID: 33493462; PMCID: PMC7836903.
[30] Baxter, J. M. S., Kavanaugh, K., & Vonderheid, S. (2014). Exploring the lived experience of trauma among obstetric registered nurses. Journal of Obstetric, Gynecologic & Neonatal Nursing, 43. https://doi.org/10.1111/1552-6909.12441
[31] Beck, C. T. (2019). Secondary traumatic stress in maternal-newborn nurses: Secondary qualitative analysis. Journal of the American Psychiatric Nurses Association, 26(1), 55–64. https://doi.org/10.1177/1078390319886358
[32] Isobel, S., & Thomas, M. (2021). Vicarious trauma and nursing: An integrative review. International Journal of Mental Health Nursing, 31(2), 247–259. https://doi.org/10.1111/inm.12953
[33] Staff, I. H. (2022, July 13). Study: 186% pandemic spike in nurse demand worsens turnover and stress. Incredible Health. Retrieved December 27, 2022, from https://www.incrediblehealth.com/blog/study-covid-19-anniversary-nurse-impact/
[34] Muir KJ, Wanchek TN, Lobo JM, Keim-Malpass J. Evaluating the Costs of Nurse Burnout-Attributed Turnover: A Markov Modeling Approach. J Patient Saf. 2022 Jun 1;18(4):351-357. doi: 10.1097/PTS.0000000000000920. Epub 2021 Oct 15. PMID: 35617593.
[35] NSI Nursing Solutions. (2022). 2022 NSI National Health Care Retention & RN Staffing Report.
[36] Schulman, M., & Menschner, C. (2018, January). Laying The Groundwork for Trauma-Informed Care. Hamilton, NJ: Center for Healthcare Strategies, Inc. Retrieved from https://www.chcs.org/media/Brief-Laying-the-Groundwork-for-TIC.pdf
[37] Schmidt J, Gambashidze N, Manser T, Güß T, Klatthaar M, Neugebauer F, Hammer A. Does interprofessional team-training affect nurses’ and physicians’ perceptions of safety culture and communication practices? Results of a pre-post survey study. BMC Health Serv Res. 2021 Apr 14;21(1):341. doi: 10.1186/s12913-021-06137-5. PMID: 33853593; PMCID: PMC8048288.
[38] Homeyer S, Hoffmann W, Hingst P, Oppermann RF, Dreier-Wolfgramm A. Effects of interprofessional education for medical and nursing students: enablers, barriers and expectations for optimizing future interprofessional collaboration – a qualitative study. BMC Nurs. 2018 Apr 10;17:13. doi: 10.1186/s12912-018-0279-x. PMID: 29643742; PMCID: PMC5891914.
[39] Swanson ML, Whetstone S, Illangasekare T, Autry AM. Obstetrics and Gynecology and Reparations: The Debt We Owe (and Continue to Accumulate). Health Equity. 2021 May 24;5(1):353-355. doi: 10.1089/heq.2021.0015. PMID: 34084987; PMCID: PMC8170721.
[40] American College of Obstetricians and Gynecologists. (2021, April). Caring for patients who have experienced trauma. ACOG. Retrieved December 28, 2022, from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2021/04/caring-for-patients-who-have-experienced-trauma
[41] Respectful maternity care framework and evidence-based clinical practice guideline. (2022). Journal of Obstetric, Gynecologic & Neonatal Nursing, 51(2). https://doi.org/10.1016/j.jogn.2022.01.001
[42] DeAndrade, S., Pelletier, A., Bartz, D., & Dutton, C. (2020). Trauma informed care training in OB/GYN residency programs [26G]. Obstetrics & Gynecology, 135. https://doi.org/10.1097/01.aog.0000664924.02840.92


2 Responses